Endothelial Cells
Endothelial cells (ECs) form the endothelium, a layer of single-cell thickness that coats the interior wall of all blood vessels including arteries, capillaries, and veins. This monolayer of cells acts as a barrier to separate the vascular lumen from surrounding tissues and regulates the passage of fluid and nutrients between the two.1
Formation and Structure
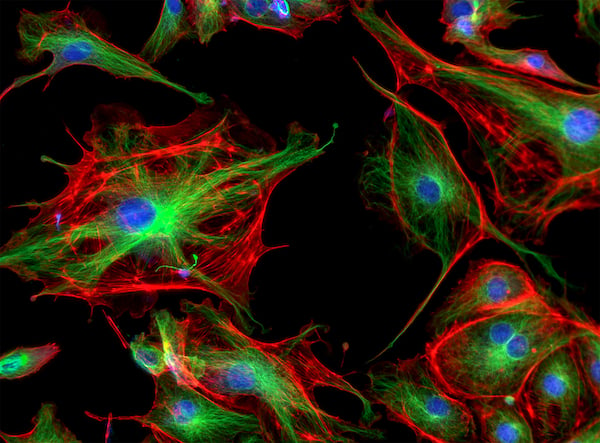
The shape and size of ECs depends on their specialization, but they are typically thin and elongated, and approximately 30-50 µm in length.2 It is thought that ECs originate from mesoderm-derived angioblasts and hemangioblasts during embryonic and adult development.3
Primordial endothelial cells specialize into tissue-specific phenotypes of arterial, venous, hemogenic, and lymphatic subtypes with distinct functions for vascular development. The forkhead box (FOX) and ETS transcription factor families have been shown to be important in endothelial specification and establishment.4 In addition, vascular endothelial growth factor (VEGF) is an angiogenic factor that regulates endothelial survival, proliferation, differentiation, and vascular permeability, and has been shown to be an important candidate for cancer therapy as it is upregulated in many tumors.5
Function
Endothelial cells form a semi-permeable barrier between the blood and surrounding tissues within all blood vessels in the body. This monolayer of cells is an important endocrine organ, and has been shown to play a major role in regulating blood fluidity, the transfer of solutes and macromolecules, immune responses and inflammation.6
Vessel permeability
Depending on their nature and function, ECs form either a continuous or porous endothelium, allowing various levels of passage of fluids and nutrients between the lumen and surrounding tissues.
Blood Flow
ECs control blood flow by initiating the vasodilation and vasoconstriction of underlying smooth muscle with the release of various vasoactive factors. Vasodilatory factors include nitric oxide (NO), prostacyclin (PGl2), and endothelium derived hyperpolarizing factor (EDHF), and vasoconstrictive factors include thromboxane (TXA2), norepinephrine, and endothelin-1 (ET-1).7 Increasing blood flow is an important part that ECs play in enhancing the delivery of leukocytes to tissues, as well as increasing the leakage of plasma proteins into the tissue and promoting the activation of neutrophils, during an inflammatory response.8
Hemostasis and Thrombosis
ECs are essential for maintaining hemostasis – the cessation of bleeding – and preventing thrombosis. A functional endothelium will release antiplatelet and anticoagulant agents to prevent platelet aggregation and fibrin formation. The endothelium also produces an active antithrombotic surface with prostacyclin to allow the smooth movement of plasma and cellular constituents through the vasculature by inhibiting platelet aggregation.9 In the event of vascular injury, ECs will activate platelet adhesion and blood coagulation with protein factor VIII, as well as platelet aggregation and fibrin formation.10 During wound healing, ECs release pro-fibrinolytic agents to degrade blood clots by fibrinolysis.
Role in Health and Disease
Vascularization relies on a highly organized developmental program, and abnormal growth can result in a dysfunctional endothelium. Aberrant endothelial cells or vasculature is often a hallmark of many diseases, including cancer, atherosclerosis and other heart diseases, retinopathy, strokes, chronic kidney failure, and many more. Assessment of endothelial cell heterogeneity can be a good indicator of health; endothelial function can predict future cardiac events in individuals with cardiovascular disease,7 and the role of ECs in angiogenesis is of particular interest to researchers studying tumor formation.
Emerging Research
Current research focuses on the role of ECs in the pathogenesis of many diseases, including viral infections such as COVID-19,11 liver disease12, and pulmonary arterial hypertension.13 Changes in EC cell marker expression have been linked to visceral obesity and insulin resistance.14 ECs have also been shown to stimulate the growth of tumors by regulating a growth-promoting microenvironment,15 which is opening up new possibilities for oncological therapeutic candidates.16
Tools To Study Endothelial Cells
EC cell markers can be identified with immunostaining methods including flow cytometry and immunocytochemistry. Enzyme-linked immunosorbent assays (ELISAs) can quantify relevant soluble compounds such as VEGF.17 Fluorochrome-labeled bromodeoxyuridine (BRdU) incorporation and CSFE dye dilution are flow cytometry-based methods that allow for single cell analysis of ECs. EC culture models can be used to replicate the physiological pressure, stretch, and shear stress of normal and pathological blood vessels.18 Gene transfer is also emerging as a useful tool for characterizing the function of individual genes and proteins in ECs.19
Cell Markers
The markers expressed by ECs can depend on the developmental stage and the tissue-specific determination. CD31, also known as PECAM-1, is constitutively expressed on ECs, and CD34 is expressed on endothelial progenitor cells but often lost during maturation.20,21 CD54 and Tek are found on vascular ECs, while LYVE-1 is expressed on the surface of lymphatic ECs. Factors regulated by endothelial cells are also good cell markers, including receptor tyrosine kinase VEGFR2 used in angiogenesis22 and von Willebrand factor (VWF), a glycoprotein involved in hemostasis.23
Overview of Specific EC Markers
| Cell Marker | Alternative Names | Location |
|---|---|---|
| CD13 | TAPN | Cell surface |
| CD29 | Integrin β1 | Cell surface |
| CD31 | PECAM-1 | Cell surface |
| CD34 | Cell surface of endothelial progenitor cells | |
| CD39 | NTPDase 1, TPDase | Cell surface |
| CD44 | Cell surface | |
| CD49a | Integrin alpha-1, VLA-1, ITGA1 | Cell surface |
| CD54 | ICAM-1, BB2 | Cell surface |
| CD73 | 5'-nucleotidase, NT5E, E5NT | Cell surface |
| CD93 | C1qR, C1QR1, MXRA4 | Cell surface |
| CD105 | Endoglin, ENG, END, ORW | Cell surface |
| CD141 | BDCA-3, TM | Cell surface |
| CD143 | ACE | Cell surface |
| CD144 | Cadherin 5, VE-cadherin | Cell surface |
| CD157 | BST-1 | Cell surface |
| CD201 | EPCR | Cell surface |
| CD309 | VEGFR2, KDR, Flk-1 | Cell surface |
| Tek | Tie-2 | Cell surface |
| LYVE-1 | Cell surface | |
| VWF | Cell surface |
References
1. Aman, J., Weijers, E. M., van Nieuw Amerongen, G. P., Malik, A. B., & van Hinsbergh, V. W. (2016). Using cultured endothelial cells to study endothelial barrier dysfunction: Challenges and opportunities. American journal of physiology. Lung cellular and molecular physiology, 311(2), L453–L466. https://journals.physiology.org
2. Krüger-Genge, A., Blocki, A., Franke, R. P., & Jung, F. (2019). Vascular Endothelial Cell Biology: An Update. International journal of molecular sciences, 20(18), 4411. https://www.mdpi.com
3. Tsuji-Tamura, K., Ogawa, M. Morphology regulation in vascular endothelial cells. Inflammation and Regeneration. 38, 25 (2018). https://inflammregen.biomedcentral.com
4. De Val, S., Chi, N. C., et al. (2008). Combinatorial regulation of endothelial gene expression by ets and forkhead transcription factors. Cell, 135(6), 1053–1064. https://www.cell.com
5. Duffy AM, Bouchier-Hayes DJ, Harmey JH. Vascular Endothelial Growth Factor (VEGF) and Its Role in Non-Endothelial Cells: Autocrine Signalling by VEGF. In: Madame Curie Bioscience Database [Internet]. Austin (TX): Landes Bioscience; 2000-2013. Available from: https://www.ncbi.nlm.nih.gov
6. Félétou M. (2011) The Endothelium: Part 1: Multiple Functions of the Endothelial Cells—Focus on Endothelium-Derived Vasoactive Mediators. San Rafael (CA): Morgan & Claypool Life Sciences. Available from: https://www.ncbi.nlm.nih.gov
7. Sandoo, A., van Zanten, J. J., et al. (2010). The endothelium and its role in regulating vascular tone. The open cardiovascular medicine journal, 4, 302–312. https://opencardiovascularmedicinejournal.com
8. Pober, J., Sessa, W. (2007). Evolving functions of endothelial cells in inflammation. Nat Rev Immunol 7, 803–815. https://www.nature.com
9. Rajendran, P., Rengarajan, T., et al. (2013). The vascular endothelium and human diseases. International journal of biological sciences, 9(10), 1057–1069. https://www.ijbs.com
10. Neubauer, K., Zieger, B. (2021) Endothelial cells and coagulation. Cell Tissue and Research. https://link.springer.com
11. Fosse JH, Haraldsen G, Falk K and Edelmann R (2021) Endothelial Cells in Emerging Viral Infections. Frontiers in Cardiovascular Medicine. 8:619690. https://www.frontiersin.org
12. Gracia-Sancho, J., Caparrós, E., Fernández-Iglesias, A. et al. (2021) Role of liver sinusoidal endothelial cells in liver diseases. Nature Reviews Gastroenterology Hepatology. 18, 411–431. https://www.nature.com
13. Colin E. Evans, Nicholas D. Cober, Zhiyu Dai, Duncan J. Stewart, You-Yang Zhao. (2021) European Respiratory Journal; 58(5). https://erj.ersjournals.com
14. Cifarelli, V., Appak-Baskoy, S., Peche, V.S. et al. Visceral obesity and insulin resistance associate with CD36 deletion in lymphatic endothelial cells. Nature Communications. 12, 3350 (2021). https://www.nature.com
15. Wei, C., Tang, M., Xu, Z. et al. Role of endothelial cells in the regulation of mechanical microenvironment on tumor progression. Acta Mechanica Sinica. 37, 218–228 (2021). https://link.springer.com
16. Solimando AG, Da Vià MC, Leone P, et al. (2021) Halting the vicious cycle within the multiple myeloma ecosystem: blocking JAM-A on bone marrow endothelial cells restores angiogenic homeostasis and suppresses tumor progression. Haematologica. 106(7):1943-1956. https://haematologica.org
17. Vernes JM, Meng YG. (2015). Detection and Quantification of VEGF Isoforms by ELISA. Methods Mol Biol. 1332:25-37. https://link.springer.com
18. Rosendo Estrada, Guruprasad A. Giridharan, et al. (2011). Endothelial Cell Culture Model for Replication of Physiological Profiles of Pressure, Flow, Stretch, and Shear Stress in Vitro. Analytical Chemistry. 83 (8), 3170-3177. https://pubs.acs.org
19. Zvonimir S. Katusic, Noel M. Caplice, and Karl A. Nath. (2003). Nitric Oxide Synthase Gene Transfer as a Tool to Study Biology of Endothelial Cells. Arteriosclerosis, Thrombosis, and Vascular Biology. 23:1990–1994. https://www.ahajournals.org
20. Mantovani, A., Dejana, E. (1998). Endothelium, Editor(s): Peter J. Delves, Encyclopedia of Immunology (Second Edition), Elsevier, 802-806, ISBN 9780122267659 https://www.sciencedirect.com
21. Murga M, Yao L, Tosato G. (2004). Derivation of endothelial cells from CD34- umbilical cord blood. Stem Cells. 22(3):385-95. https://academic.oup.com
22. Ferrara N, Gerber HP, LeCouter J. (2003). The biology of VEGF and its receptors. Nature Medicine. 9(6):669-76. https://www.nature.com PMID: 12778165
23. Pusztaszeri MP, Seelentag W, Bosman FT. (2006) Immunohistochemical Expression of Endothelial Markers CD31, CD34, von Willebrand Factor, and Fli-1 in Normal Human Tissues. Journal of Histochemistry & Cytochemistry. 54(4):385-395. https://journals.sagepub.com

