Epithelial Cells
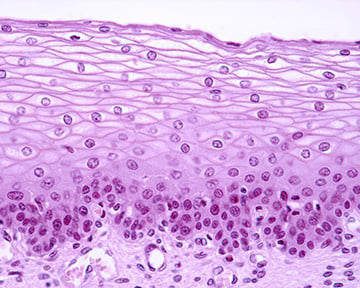
Epithelial cells are a diverse group of tightly packed cells that form a physical barrier by lining the cavities of the major organs – the skin, lungs, gastrointestinal tract, and genitourinary system – separating them from one another and the external environment.
Formation and structure
Epithelia can originate from all three embryonic germ layers – the ectoderm, the mesoderm, and the endoderm. For example, keratinocytes have an ectodermal origin, the cells that form the lining of the gastrointestinal tract develop from the endoderm, and the lining of body cavities originate from the mesoderm. Since the epithelium develops from rapidly dividing stem cells, it is also a major site for carcinogenesis.1
Formation of the epithelium begins as a single layer of cells adherent to the basement membrane, which further matures as growth factors and extracellular matrix are deposited at its interface with the underlying mesenchyme. Multiprotein complexes, including transmembrane integrin heterodimers, enable the adhesion of basal epithelial cells to the underlying basement membrane. Intercellular communication is achieved by the formation of adherent and tight junctions, along with desmosomes, and this enables numerous cells to function as one entity. These intercellular junctions also assist in distinguishing the apical, basal, and lateral surfaces of the cells, which is essential for establishing epithelial cell polarity.2
Epithelia can be classified into several types based on their thickness, specialized function, and location, however, they share several molecular and cellular characteristics. These can be further described as being protective, secretory, or absorptive, depending on their predominant property, but often all three functions coexist. Epithelia are classified according to their shape and the number of layers:
- Cell shape: squamous, cuboidal, and columnar
- Cell layers: simple (one layer) or stratified (multiple layers)
- Specialized epithelium: ciliated, transitional, and glandular
Function
The physical barrier of epithelium confers important protective and regulatory functions, including secretion, selective absorption, transcellular transport, and sensory perception. Epithelia also recruit or activate other specialized effector cells and contribute to innate immunity. For example, they rely on eosinophils to initiate and augment immune responses and exert anti-inflammatory effects. Evidence also suggests that there are similarities between certain polypeptides secreted by epithelial cells and neutrophils, including lysozymes, lactoferrin, and defensins. This can be attributed to the co-expression of genes directing the production of these antimicrobial substances by both cell types.3
Most epithelial cells renew throughout life and the timing of the replacement of cells varies among different epithelia. For example, the epithelium of the intestine renews every five days, while the epidermis takes four weeks to restore. The process of renewal is attributed to the presence of multipotent stem cells. Derived from these, epithelial stem cells are specified during development and are controlled by epithelial-mesenchymal interactions.2
Epithelial to mesenchymal transition (EMT) is a unique cellular process that occurs when epithelial cells lose their polarity and adhesion properties, and acquire mesenchymal phenotypes in response to changes in gene expression and post-translational regulation. This modification gives epithelial cells unique invasive and migratory properties, and they transform into mesenchymal stem cells. This process is known to be crucial for physiological processes such as embryogenesis, wound healing, but also pathological processes including development of metastasis. The identification of the signaling pathways that lead to the activation of EMT can provide new insights into the plasticity of cellular phenotypes and possible therapeutic interventions.2
Emerging research
Recent clinical and preclinical trials indicate that various types of stem cells can be used to support the regeneration or recovery of lost neurons in the management of neurodegenerative diseases. The use of human amniotic epithelial cells may be a promising approach for cell-based therapies in the future, not least because this represents less risk of tumorigenicity or immunogenicity, and there are no ethical concerns.4
Tools to study epithelial cells
Cell markers
Cell markers can be used to study epithelial cell biology including embryonic development, carcinogenesis, and EMT status. Traditional epithelial markers are epithelial membrane antigen (EMA/MUC1) and pan-cytokeratin, although EMA is not produced by all epithelia. The loss of epithelial markers is also associated with EMT and metastatic progression in certain carcinomas.5 Epithelial cells can be identified by the expression of the following:
Cell Adhesion Molecules: The epithelium-specific antigen or Epithelial Cell Adhesion Molecule (EpCAM) is expressed by most healthy epithelial cells, but is not seen in mucous squamous epithelia like those in the upper airways and intestine; E-cadherin is expressed on all epithelial cells except neuronal epithelium.
Cytokeratins: These can be organized into two distinct subgroups, including the acidic (type A, 9-20) and the basic cytokeratins (type B, 1-8), and are generally found in heterodimeric pairs consisting of one of each subtype. Epithelial cells express a tissue- or organ-specific cytokeratin profile that can be used to identify individual epithelia, for example, cytokeratin 15 is a marker of hair follicle stem cells.5,6
CD66f or pregnancy-specific beta-1 glycoprotein (PSBG-1) is produced by the placental syncytiotrophoblast, fetal liver, and myeloid cell lines. It is found abundantly in maternal serum during late pregnancy, and is thought to protect the fetus from the maternal immune system.7
| Surface marker | Alternative names | Location |
|---|---|---|
| CD66e | CEACAM5, member of the CEA gene family | Surface, post-birth only found in tumor cells |
| CD66f | PSBG-1, member of the CEA gene family | Surface |
| CD340 | HER2/erbB2, MLN 19 | Surface |
| CD331 | FGFR1, BFGFR, FLT-2 | Surface |
| CD324 | E-Cadherin, CDH1 | Surface |
| CD326 | EpCAM, EGP314 | Surface |
| CD318 | CDCP1, SIMA135, TRASK, gp140 | Surface |
| CD249 | EAP, BP-1, glutamyl aminopeptidase | Surface |
| CD118 | LIFR, Leukemia inhibitory factor receptor alpha | Surface |
References
1. Hinck, L., Näthke, I. (2014). Changes in cell and tissue organization in cancer of the breast and colon. Current opinion in cell biology, 26, 87–95. https://doi.org/10.1016/j.ceb.2013.11.003
2. Yang, J., Antin, P., et al. (2020) Guidelines and definitions for research on epithelial-mesenchymal transition. Nat Rev Mol Cell Biol. 2:41–352. DOI: https://doi.org/10.1038/s41580-020-0237-9
3. Ganz T. (2002). Epithelia: not just physical barriers. Proceedings of the National Academy of Sciences of the United States of America. 99(6). https://doi.org/10.1073/pnas.072073199
4. Huiming Xu, Jiaofei Zhang, et al. (2019). Therapeutic potential of Human Amniotic Epithelial cells on Injuries and Disorders in the Central Nervous System. Stem Cells International. DOI: https://doi.org/10.1155/2019/5432301
5. Guislaine Barriere, Pietro Fici, et al. (2014). Circulating tumor cells and epithelial, mesenchymal and stemness markers: characterization of cell subpopulations. ATM. 2:11. DOI: 10.3978/j.issn.2305-5839.2014.10.04
6. Zeisberg M, Neilson EG. (2009). Biomarkers for epithelial-mesenchymal transitions. J Clin Invest. 119(6):1429-37. doi: 10.1172/JCI36183.
7. Stockinger, H., Majdic, O., et al. (2003). Monoclonal Antibodies to Human Cell Surface Antigens. Current protocols in immunology, 53(1), A.4A.1–A.4A.49. https://doi.org/10.1002/0471142735.ima04as53

