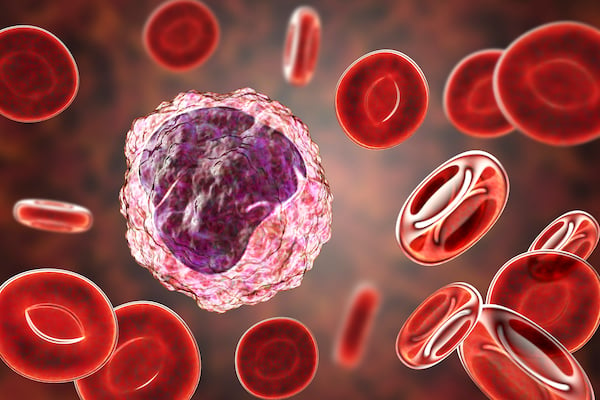
Monocytes
Monocytes are a type of leukocyte that circulates in the bone marrow, spleen, and blood, comprising approximately 10% of total leukocytes in humans, and 2-4 % in mice.1 Monocytes are broadly divided into three subsets – classical, intermediate, and non-classical – and show vast heterogeneity in function and surface protein expression. Classical monocytes have a high capacity for phagocytosis, migration and innate immune responses.2 They can also differentiate into monocyte-derived dendritic cells (DCs) to bridge innate and adaptive immune responses, or into macrophages upon tissue migration.2 Intermediate monocytes have elevated capacity to secrete inflammatory mediators and specialize in antigen presentation, while non-classical monocytes engage in FcR-mediated phagocytosis and are responsible for the anti-viral responses of this lineage.2
Formation
Hematopoietic stem cells in the bone marrow develop into a common myeloid progenitor, which matures through a series of steps into either erythrocytes, platelets, basophils, neutrophils, eosinophils, or monocytes. It is thought that classical monocytes develop first, and then the non-classical type, with the intermediate subset characterizing a transition state. However, a specific progenitor lineage for non-classical monocytes may also exist.3 They can remain in circulation for up to two days as sentinels, waiting to be recruited into tissues in response to stimuli, but otherwise die and are removed.
Monocytes are recruited from the bloodstream into surrounding tissues, where – through regulation primarily by colony-stimulating factor 1 (CSF-1)1, 4 – they give rise to macrophages or DCs. They are able to repopulate tissue macrophage populations, then adopt similar gene expression and perform their specific functions.4
Function
Monocytes are known to play a central role in both innate and adaptive immunity. Circulating monocytes replenish tissue macrophages and DCs in steady-state conditions, and at increasing rates during inflammation, helping to maintain homeostasis by secreting cytokines that attract other immune cells. They also have direct anti-pathogenic activity through phagocytosis, antigen processing and presentation, and the production of reactive oxygen species, nitric oxide, myeloperoxidase, and inflammatory cytokines.1, 4 Furthermore, monocytes can trigger and polarize T cell responses, and enter lymph nodes during infection to promote adaptive immune responses.1, 5
Monocytes are therefore essential components of the immune response, but they also contribute to the pathogenesis of many chronic inflammatory conditions and degenerative diseases. They have been shown to infiltrate the colon in inflammatory bowel diseases – such as Crohn's and ulcerative colitis – the joints in rheumatoid arthritis, lesions in multiple sclerosis, the heart following myocardial infarction, and some cancer tumors.6
The function of monocytes – and monocyte-derived cells – in tumor formation and progression is complex, and phenotypically similar cells have even been shown to perform opposing roles.3 Monocytes can directly kill malignant cells through phagocytosis and tumoricidal mediators. Conversely, they may also regulate angiogenesis and help to remodel the extracellular matrix of tumor cells.3 Classical monocytes are also believed to be a primary source of tumor-associated macrophages (TAMs) that enable growth and seeding of tumor cells.3
Emerging Research
Various cytokines associated with monocytes are of interest to develop novel therapeutic strategies. CSF-1, for example, is a potential candidate for cancer immunotherapies because of its regulatory action in the differentiation of TAMs. Inhibition of cytokine receptor CCR2 – which mediates the movement of monocytes from the bone marrow into peripheral blood, and recruitment to tumor sites – has been shown to reduce tumor growth in mouse models.7 Additionally, blocking their recruitment into tissues has resulted in a reduction of inflammation in mouse models of colitis, peritonitis, and atherosclerosis.6 Monocyte abundancy in peripheral blood is also discussed as a biomarker to improve cancer diagnosis and treatment strategies in hematological malignancies such as B cell lymphoma, as well as cervical cancer.7
Tools to Study Monocytes
Monocytes are commonly studied by flow cytometry from fresh blood samples to minimize cell transformation and marker upregulation. Preparation includes lysing of red blood cells and labeling with fluorochrome-conjugated antibodies, often with intermediate and final washing steps to improve data resolution. Using staining kits – such as DURAClone IF Monocyte Activation – enables streamlined analysis of both surface markers and the expression of proinflammatory TNFα in a no-wash analysis mode.8
Cell Markers
Most surface markers are not exclusive to monocytes, and therefore multiple markers should be chosen to increase study robustness.6 Monocyte subsets were originally identified by their expression of CD14 and CD161, however studies are on-going to further characterize the specific markers associated with each subtype.9, 10
- Classical (CM) – high CD14 and no CD16
- Intermediate (IM) – high CD14 and low CD16
- Non-classical (NCM) – low CD14 and high CD16
| Cell Marker | Alternative Names |
|---|---|
| CD11b | ITGAM |
| CD11c | ITGAX |
| CD33 | p67, Sialic acid-binding Ig-like lectin 3 (SIGLEC3) |
| CD36 | Glycoprotein IIIb, GP3B, GP4, GPIV, PASIV, SCARB3 |
| CD43 (mice only) | Leukosialin, Galactoglycoprotein, Leukocyte sialoglycoprotein, SPN, GPL115, LSN |
| CD45 | Leukocyte common antigen, L-CA, PTPRC |
| CD62L | L-selectin, SELL, LAM1, LECAM1, LYAM1, Leu-8 |
| CD64 | IgG Fc receptor I, FCGR1A, IGFR1 |
| CD74 | DHLAG, Ia-GAMMA, HLADG |
| CD86 | CD28LG2, B7-2, LAB72 |
| CD120a | TNF Receptor I |
| CD120b | TNF Receptor II, TNFRSF1B |
| CD163 | GHI/61, M130, RM3/1, p155 |
| CD172a | SHPS-1, SIRPA, PTPNS1 |
| CD184 | CXCR4 |
| CD192 | CCR2 |
| CD195 | CCR5 |
| CD281 | Toll-like receptor 1, TLR1 |
| CD282 | Toll-like receptor 2, TLR2 |
| CD284 | Toll-like receptor 1, TLR4 |
| CD300e | IREM-2, CMRF35-A5, LMIR6 |
| CX3CR1 | CCRL1, CMKBRL1, CMKDR1, GPR13, GPRV28, V28, C-X3-C motif chemokine receptor 1 |
| HLA-DR |
References
1. Italiani P, Boraschi D. (2014) From Monocytes to M1/M2 Macrophages: Phenotypical vs. Functional Differentiation. Front Immunol. 5:514. https://www.frontiersin.org
2. Kapellos TS, Bonaguro L et al. (2019) Human Monocyte Subsets and Phenotypes in Major Chronic Inflammatory Diseases. Front. Immunol. 10:2035. https://www.frontiersin.org
3. Olingy CE, Dinh HQ et al. (2019) Monocyte heterogeneity and functions in cancer. J Leukoc Biol. 106(2):309-322. https://jlb.onlinelibrary.wiley.com
4. Serbina NV, Jia T et al. (2008) Monocyte-mediated defense against microbial pathogens. Annu Rev Immunol. 26:421-452. https://www.annualreviews.org
5. Shi C, Pamer EG. (2011) Monocyte recruitment during infection and inflammation. Nat Rev Immunol. 11(11):762-774. https://www.nature.com
6. Coillard A, Segura E. (2019) In vivo Differentiation of Human Monocytes. Front Immunol. 10:1907. https://www.frontiersin.org
7. Olingy CE, Dinh HQ et al. (2019) Monocyte heterogeneity and functions in cancer. J Leukoc Biol. 106(2):309-322. https://jlb.onlinelibrary.wiley.com/doi
8. Monneret G, Demaret J et al. (2017) Novel Approach in Monocyte Intracellular TNF Measurement: Application to Sepsis-Induced Immune Alterations. Shock. Mar;47(3):318-322. https://journals.lww.com PMID: 27513085
9. Ong S-M, Teng K et al. (2019) A Novel, Five-Marker Alternative to CD-16-CD14 Gating to Identify the Three Human Monocyte Subsets. Front. Immunol. 10:1761. https://www.frontiersin.org
10. Merah-Mourah F, Cohen SO et al. (2020) Identification of Novel Human Monocyte Subsets and Evidence for Phenotypic Groups Defined by Interindividual Variations of Expression of Adhesion Molecules. Sci Rep 10:4397. https://www.nature.com

